Endometriosis is a medical condition where cells like those lining your uterus (womb) are found in other parts of your body. Every month these cells react like your womb lining, building up and then breaking away. This inflames the surrounding tissues, causing pain which is often worse just before and during your period.
If you have endometriosis, you’re not alone. About one in every 10 women is affected. It mostly affects women of childbearing age and usually disappears after the menopause. Endometriosis is often a long-term condition, with no simple cure. But there are treatments which can help.
Click here to find out more about our Specialist Endometriosis Clinic
About endometriosis
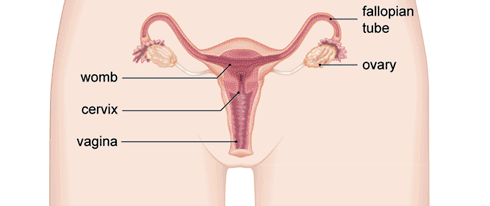
Normally, as part of the menstrual cycle, your womb lining thickens every month to receive a fertilised egg. If an egg doesn’t get fertilised (if you don’t get pregnant), the lining of your womb breaks down. This lining leaves your body as menstrual blood (a period). This process is controlled by your body’s hormones.
In endometriosis, you have cells like those that would normally line your womb (endometrial tissue) elsewhere in your body. This tissue will also thicken, break down and bleed with your menstrual cycle, but this tissue and blood has no way of leaving your body. This can lead to pain, swelling and scarring.
Endometriosis usually affects the tissues inside your pelvis and is most common between the womb and the rectum (back passage). It’s also common on the ligaments attached to the back of the womb. If you have endometriosis on your fallopian tubes or ovaries, it can lead to fertility problems. Endometriosis can affect other parts of your body, such as your lungs, but this is rare.
Symptoms of endometriosis
One of the most common symptoms of endometriosis is pelvic pain which is usually worse just before, and during your period. The pain may get worse over time and you may find that it’s not eased by taking over-the-counter painkillers such as ibuprofen.
Other typical symptoms include pain during sex and heavy bleeding during your periods. If you’re trying for a baby you may find that you have difficulties becoming pregnant. You may feel extremely tired. Some women become depressed because of the long-term pain they have.
There are some less common symptoms. Endometriosis on your bowel can cause pain when you have a bowel movement. You may also have blood in your faeces during your period. If you have endometriosis on your bladder, it can cause pain when you pass urine. You may also see blood in your urine.
All these symptoms may be caused by things other than endometriosis. If you have any of these symptoms, see your GP. Symptoms of endometriosis often ease during pregnancy, and usually get better or disappear after the menopause.
Some women have no symptoms at all. You may only find out that you’ve got endometriosis after having tests for other conditions, for instance for infertility.
Diagnosis of endometriosis
Your consultant will ask you about your symptoms. Don’t be embarrassed to tell them about the problems you’re having – including pain during sex, or seeing blood when going to the toilet. It’s important that they know about these.
Your consultant may offer you the following tests:
- A vaginal or rectal examination. A vaginal examination involves your GP inserting gloved, lubricated fingers into your vagina to gently feel for any abnormalities in and around your uterus (womb). At the same time, they’ll use their other hand to lightly press on your abdomen (tummy). A rectal examination involves your GP inserting a gloved, lubricated finger into your anus (back passage). This may feel uncomfortable but shouldn’t be painful. Let your consultant know if anything hurts. You can ask to have someone stay with you while your GP does these tests, if you prefer.
- An ultrasound scan. Ultrasound uses sound waves to produce an image of the inside of the body. To look for endometriosis, an ultrasound scan may be done using a sensor placed in your vagina. An ultrasound scan may be helpful in picking up other causes of your symptoms. It doesn’t always pick up endometriosis, even if you have it.
Click here for more information on Diagnosing Endometriosis
Treatment of endometriosis
About one in three women get better on their own over 6 to 12 months. Other women may need to have treatment to reduce their symptoms. Your treatment will depend on factors such as how bad your symptoms are and whether or not you want to have children.
A number of treatments can help to manage your symptoms, but they don’t always work in the long-term. About half of women find that their symptoms come back. You may choose to have another course of medication or more surgery if this happens.
Your consultant will discuss the various options with you, and help you decide which treatment is best for you.
Pain medicines
Your doctor will probably suggest that you try a non-steroidal anti-inflammatory medicine such as ibuprofen to ease pain and discomfort. You can buy these over-the-counter medicines from your pharmacy. Paracetamol is an alternative. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
Hormone treatments
Hormone treatments can help to ‘damp down’ or suppress endometriosis and so lessen your pain. They aren’t suitable for treating endometriosis in women who are trying to become pregnant.
If you’re not trying to get pregnant, your consultant may offer you the combined oral contraceptive pill. This may be for a few months at first, but if it’s helpful, you’ll usually be able to carry on taking it.
If that doesn’t help, or doesn’t suit you, there are several other types of hormonal treatment that your doctor may offer you. These include:
- Progestogens – which can be given orally (tablets), as an injection every three months or in an intrauterine system (‘coil’).
- gonadotrophin-releasing hormone (GnRH) agonists – These may be given by injection, but may also be given as a nasal spray or in an implant.
Each of these medicines has different side-effects and there may be limits on how long you can take them without a break. Your doctor can explain these and discuss with you which treatment may be best for you.
Surgery
Surgery can remove areas of endometriosis. This can help to improve your chance of getting pregnant if your endometriosis is affecting your fertility, and can also reduce your pain. Surgery for endometriosis is done under a general anaesthetic so you’ll be asleep. Endometriosis can come back after surgery, so you may need to have surgery again in the future.
Laparoscopy (keyhole surgery)
Surgery can often be done by laparoscopy – a type of keyhole surgery. This involves a gynaecologist looking inside your abdomen (tummy) using a narrow, tube-like telescopic camera (laparoscope) inserted through a small cut. They can then remove or destroy any patches of endometriosis.
Laparotomy (open surgery)
If you have severe endometriosis, keyhole surgery may not be suitable. You may need an operation called a laparotomy where a larger cut is made in your abdomen, usually along the bikini line. If your gynaecologist recommends this they will explain the procedure and why it’s best for you.
Hysterectomy
If you don’t want to have children in the future, your gynaecologist may offer you a hysterectomy. This is a larger operation to remove your womb and sometimes your ovaries. This operation can also be done by keyhole surgery.
